Jaundice Disease - Symptoms, Causes, Complications and Prevention
Jaundice meaning
Jaundice disease, also known as hyperbilirubinemia, is a condition characterised by a yellow discoloration of the body tissue (skin, eye sclera, and mucous membranes) resulting from the deposition of excess bilirubin, a yellow-orange bile pigment formed by breakdown of red blood cells and secreted by the liver. This indicates increased production, impairment of uptake, conjugation, and excretion of unconjugated or conjugated bilirubin from damaged hepatocytes or bile ducts. Jaundice has many causes, including hepatitis, gallstones, and tumours.
Elevation of unconjugated or conjugated bilirubin can result in jaundice. Normal serum levels of bilirubin are less than 1 milligram per deciliter (mg/dL),
when serum bilirubin levels exceed 3 mg/dL, the patient will have scleral icterus (yellow discoloration of the eye sclera). There will be progressively more discolouration ranging from lemon yellow to apple green, especially if the serum bilirubin levels (hyperbilirubinemia) is further increased or long-standing. The prevalence of jaundice varies by patient population; new-borns and the elderly are more likely to be affected. Jaundice affects about 20% of full-term infants in their first week of life, most often because of a lack of development in the hepatic conjugation process.
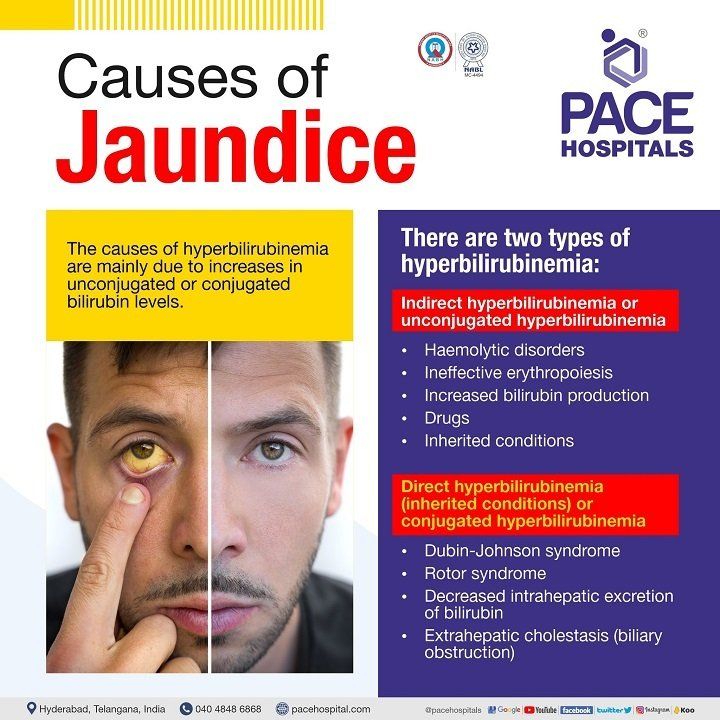
Causes of jaundice disease or hyperbilirubinemia
Hyperbilirubinemia or jaundice causes are mainly due to increases in unconjugated or conjugated bilirubin levels due to a problem with the liver, pancreas or gallbladder. In general, bilirubin has two components: unconjugated (indirect) bilirubin, which is water insoluble, present in the blood stream, bound to albumin (plasma protein) and cannot be directly excreted from the body.
Hence, it (unconjugated bilirubin) travels to the liver, combines with glucuronic acid, and converted into water soluble conjugated (direct) bilirubin (catalysed by bilirubin uridine diphosphate-glucuronosyl transferase; UDPGT) which is later excreted into the duodenum or small intestine through bile.
Causes of Jaundice disease or hyperbilirubinemia are mainly classified into two categories:
- Indirect hyperbilirubinemia or unconjugated hyperbilirubinemia
- Direct hyperbilirubinemia or conjugated hyperbilirubinemia
Indirect hyperbilirubinemia or unconjugated hyperbilirubinemia - An increase in unconjugated bilirubin (unconjugated hyperbilirubinemia) in the serum results from overproduction, impaired uptake or conjugation of bilirubin. It is due to the following:
- Haemolytic disorders
- Ineffective erythropoiesis
- Increased bilirubin production
- Massive blood transfusion
- Resorption of haematoma
- Drugs such as Rifampin, Probenecid, Ribavirin, Protease inhibitors (Atazanavir, Indinavir)
- Inherited conditions
- Crigler-Najjar types I and II
- Gilbert’s syndrome
Direct hyperbilirubinemia (inherited conditions) or conjugated hyperbilirubinemia - An increase in conjugated bilirubin (conjugated hyperbilirubinemia) is due to decreased excretion of bilirubin into the bile ducts. It is due to the following:
- Dubin-Johnson syndrome
- Rotor syndrome
- Decreased intrahepatic excretion of bilirubin
- Extrahepatic cholestasis (biliary obstruction)
Indirect hyperbilirubinemia or unconjugated hyperbilirubinemia
Haemolytic disorders: These disorders cause excessive haeme production, which may be either inherited (sickle cell anaemia, thalassemia, and deficiency of red cell enzymes such as pyruvate kinase, spherocytosis and glucose-6-phosphate dehydrogenase) or acquired (microangiopathic haemolytic anaemia, paroxysmal nocturnal haemoglobinuria, spur cell anaemia, immune haemolysis, and parasitic infections such as malaria and babesiosis). In these conditions, the serum bilirubin level rarely exceeds 5 mg/dL (86 μmol/L). The presence of renal or hepatocellular dysfunction or acute haemolysis in addition to the haemolytic disorders elevates the bilirubin levels.
Ineffective erythropoiesis: Due to deficiencies in cobalamin, iron and folate, ineffective erythropoiesis (process of red blood cell formation) occurs, resulting in increased unconjugated bilirubin concentrations.
Increased bilirubin production: large blood transfusions and resorption of haematomas (partially clotted blood or clotted blood under the skin) can both cause increased haemoglobin release and bilirubin overproduction.
Drugs: Certain medications, such as anti-tuberculosis and uricosurics (drugs that increase the excretion of uric acid), can produce unconjugated hyperbilirubinemia by decreasing bilirubin uptake in the liver.
Inherited conditions: Impaired bilirubin conjugation are caused by three different hereditary conditions: types I and II of the Crigler-Najjar syndrome, and Gilbert's syndrome.
- Crigler-Najjar type I:
Severe jaundice (bilirubin >20 mg/dL [>342 mol/L]) and neurologic impairment owing to kernicterus commonly results in death in infancy or childhood, where in these patients, UDP-glucuronosyltransferase, activity is completely absent, thereby, preventing the formation of conjugate bilirubin; and hence the inability to excrete the bilirubin into bile. It is an extremely rare neonatal illness characterised by severe jaundice (bilirubin >20 mg/dL [>342 μmol/L]) and neurologic impairment owing to kernicterus characterise this highly rare neonatal sickness, which commonly results in death in infancy and childhood.
- Crigler-Najjar type II: It is more common than type I. In these patients, mutations in the bilirubin UDPGT gene cause a reduction (typically ≤10%) of the UDPGT enzyme’s activity, which converts unconjugated bilirubin to conjugated bilirubin. Patients with this disease live into adulthood with serum bilirubin levels of 6–25 mg/dL (103–428 μmol/L).
- Gilbert's syndrome: It is a very common condition marked by poor bilirubin conjugation as a result of decreased bilirubin UDPGT activity. Gilbert's syndrome patients have moderate unconjugated hyperbilirubinemia, with serum levels almost invariably less than 6 mg/dL (103 μmol/L).
Direct hyperbilirubinemia (inherited conditions) or conjugated hyperbilirubinemia
Elevated conjugated hyperbilirubinemia is present in two rare hereditary disorders: Dubin-Johnson syndrome and Rotor syndrome. Asymptomatic jaundice disease is prevalent in patients with either disease. A decrease in intrahepatic excretion and extrahepatic (bile ducts present outside the liver) obstruction can also lead to the blockage of the bile flow into the small intestine.
Dubin-Johnson syndrome: the existence of mutations in the MRP2 gene, leading to an alteration in the bilirubin excretion into the bile ducts.
Rotor syndrome: The lack of the major hepatic drug reuptake transporters OATP1B1 and OATP1B3 causes Rotor syndrome.
Decreased intrahepatic excretion of bilirubin:
The impaired excretion of bilirubin via the hepatobiliary system is due to presence of:
- Hepatic crisis in sickle cell disease
- Pregnancy
- Viral hepatitis (A, B & D), cirrhosis, alcoholic hepatitis, non-alcoholic steatohepatitis (NASH), Epstein-Barr virus (EBV) or human herpesvirus 4, Cytomegalovirus (CMV) infection, Herpes simplex virus (HSV), Wilson's disease, and autoimmune hepatitis.
- Cholestatic liver disease, such as primary biliary cholangitis (an inflammation of the bile duct system), primary sclerosing cholangitis, biliary cirrhosis.
- Infiltrative diseases such as amyloidosis, langerhans cell histiocytosis, sarcoidosis, tuberculosis.
- Sepsis, Hypoperfusion and shock states
- Total parenteral nutrition
- Drug induced such as oral contraceptives, steroids, herbal remedies, arsenic are examples of drugs and toxins.
Extrahepatic cholestasis: It is also known as obstructive cholestasis, and it occurs due to excretory block outside the liver, along with the extrahepatic bile ducts (small tubes that carry bile from the liver and gallbladder to the small intestine, located outside the liver), which is due to presence of
- Choledocholithiasis (bile duct stones or gallstones in the common bile duct)
- Tumours such as cholangiocarcinoma (a group of cancers that begin in the bile ducts), head of pancreas cancer etc
- Extrahepatic biliary atresia (a blockage in the tubes (ducts) that carry bile from the liver to the gallbladder)
- Acute and chronic pancreatitis
- Strictures or narrowing of extrahepatic ducts
- Parasitic infections such as ascaris lumbricoides, liver flukes
- Gallbladder cancer
In children, Hepatitis A was noted to be the most common cause of jaundice, while bile duct stones, drug-induced liver disease, and malignant biliary blockage are common in the elderly. Men are more likely than women to have alcoholic and non-alcoholic cirrhosis, pancreatic cancer, chronic hepatitis B or sclerosing cholangitis. Women, on the other hand, have a higher incidence of gallbladder stones, gallbladder cacner, and primary biliary cirrhosis.
Request an appointment for Jaundice Disease treatment
Jaundice disease treatment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
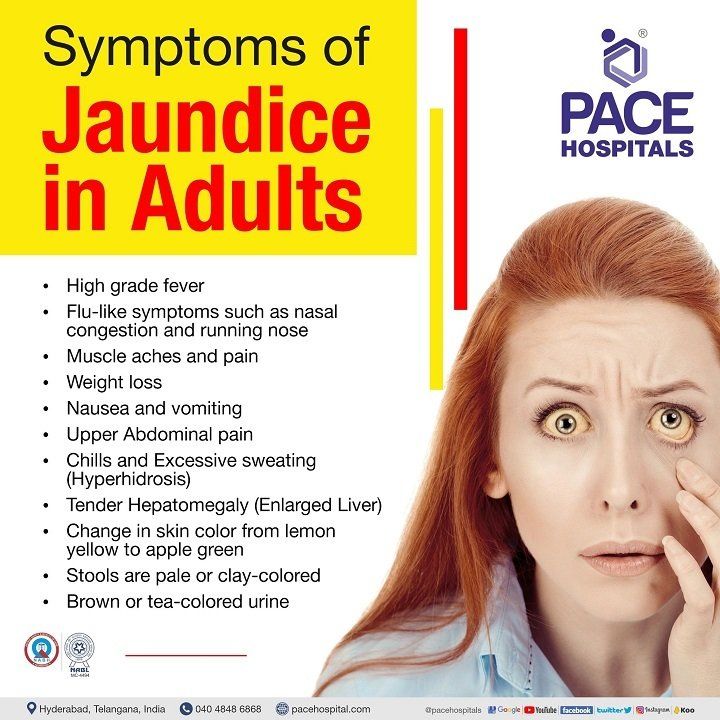
Symptoms of Jaundice disease
Jaundice symptoms are based on its underlying causes and severity. If the jaundice is caused by an infection, it will be short term. In the other case, if it is caused by liver diseases such as chronic hepatitis, the symptoms persist until the underlying cause has been treated. In some cases, the patient will be asymptomatic. Symptoms of jaundice in adults may include:
- High grade fever
- Flu-like symptoms such as nasal congestion and running nose
- Muscle aches and pain
- Weight loss
- Nausea and vomiting
- Upper Abdominal pain
- Chills and Excessive sweating (Hyperhidrosis)
- Tender Hepatomegaly (Enlarged Liver)
- Change in skin color from lemon yellow to apple green
- Stools are pale or clay-colored
- Brown or tea-colored urine
Unconjugated hyperbilirubinemia symptoms: Patients with unconjugated hyperbilirubinemia are asymptomatic, however in patients with Gilbert syndrome, nonspecific symptoms can be observed such as fatigue, abdominal cramps, and malaise.
Obstructive jaundice symptoms: Patients with biliary obstruction may present with multiple signs and symptoms, including:
- Fever
- Pruritus (skin itching)
- Abdominal pain
- Weight loss
- Muscle wasting
- Dark urine
- Pale stools
Risk factors of Jaundice disease
The jaundice risk factors are similar to the ones for liver and gallbladder problems. They could include:
- Patients with alcohol-liver diseases
- Usage of illicit drugs
- Consumption of medications that can cause live diseases
- Exposure to viral infections like hepatitis(A-C)
- Being exposed to particular industrial chemicals such as vinyl chloride that might damage liver cells
- Consumption of alcohol for a long time

Types of Jaundice disease or hyperbilirubinemia
Type of Jaundice disease is manly categorised based on their location within the liver's bilirubin uptake and excrete processes are being altered.
- Pre-hepatic jaundice
- Hepatocellular jaundice
- Post-hepatic jaundice
- Pre-hepatic jaundice: Pre-hepatic jaundice occurs when the liver's ability to conjugate bilirubin is overwhelmed by the body's excessive breakdown of red blood cells due to the presence of blood disorders or underling diseases. The haeme released from the lysate RBC undergoes a series of events in the reticuloendothelial cells of the spleen, liver, and bone marrow to generate unconjugated bilirubin. The greater the release of haeme, the more excess unconjugated bilirubin will be released, leading to hyperbilirubinemia.
- Hepatocellular jaundice or intrahepatic jaundice: Hepatocellular jaundice is caused due to parenchymal liver disease, where the liver loses the ability to conjugate bilirubin. In addition to this, a cirrhotic liver can clog and obstruct the biliary system by compressing the intra-hepatic branches of the biliary tree.
- Post-hepatic jaundice: Post-hepatic jaundice is caused by a biliary system blockage, which prevents bilirubin from being excreted into the small intestine, leading to hyperbilirubinemia.
Jaundice in pregnancy
Intrahepatic Cholestasis of Pregnancy: The most frequent pregnancy-related liver condition is intrahepatic cholestasis (ICP), which has an incidence rate of 0.2 to 2%. Bile acids normally move from the liver to the intestines to aid in digestion. In ICP, bile acids do not flow properly and build up in the body, which can cause jaundice. Patients with a history of ICP, chronic liver illness, chronic hepatitis C, multifetal pregnancy, and advanced maternal age have a greater recurrence rate of 60 to 70%. Genetic predisposition and reproductive hormones (oestrogen) have been identified as the primary contributing factors to the development of ICP.
The presence of pruritus in the third trimester, along with high maternal total serum bile acids (more than 10 micromol/L) and no other diagnoses that cause an increase in total serum bile, assists the physician in diagnosing ICP. In severe cholestasis, serum bile acid levels above 40 micromol/L increase the risk of foetal problems. Other liver function tests, such as modestly increased (no more than twice the upper limit of normal in pregnancy) alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Ursodeoxycholic acid (UDCA) is the preferred treatment for ICP.
Complication of jaundice in pregnancy: The maternal bile acids being transferred through the placenta to the foetus and accumulating in the amniotic fluid leads to complications such as:
- Sudden intrauterine demise
- Meconium-stained amniotic fluid
- Spontaneous preterm birth
- Iatrogenic preterm birth
- Neonatal ICU admission
Jaundice diagnosis: The diagnosis of jaundice depends on the laboratory evaluation to determine the cause of the disease. In order to understand the underlying cause, the gastroenterologist might ask for the following laboratory evaluation tests:
- Liver function test (LFT)
- Alanine transaminase (ALT)
- Aspartate transaminase (AST)
- Gamma -glutamyl transferase
- Alkaline phosphatase (ALP)
- Serum bilirubin
- Prothrombin time/INR
- Complete blood count (CBC)
- Urine bilirubin
- Serum or urine drug screen
- Serum lipase
- Serum acetaminophen
Hepatocellular workup:
- Viral serological test
- Autoimmune hepatitis
- Antimitochondrial antibodies
- Blood alcohol
- Genetic and iron studies
- Copper tests
Cholestatic workup:
Treatment of Jaundice disease
Jaundice treatment does not normally necessitate therapy in adults, as it is a more serious disease in neonates. However, jaundice causes and complications can be treated in severe cases. In neonates, depending on the severity of the issue, there are numerous therapies available, such as:
For unconjugated jaundice in neonates:
- Phototherapy
- Pharmacological agents such as immunoglobulin therapy
- Exchange transfusion
For conjugated jaundice neonates:
- Surgical procedure includes Kasai procedure
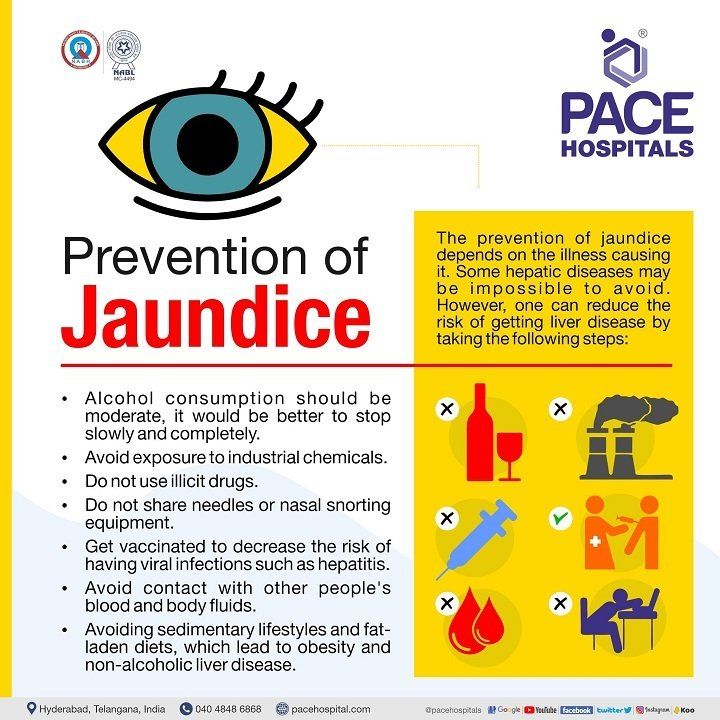
Prevention of Jaundice disease
The prevention of jaundice depends on the illness causing it. Some hepatic diseases may be impossible to avoid. However, one can reduce the risk of getting liver disease by taking the following steps:
- Alcohol consumption should be moderate, it would be better to stop slowly and completely.
- Avoid coming into contact with industrial chemicals.
- Stop using illicit drugs.
- Never exchange needles or nasal snorting supplies.
- Get vaccinated to decrease the risk of having viral infections such as hepatitis.
- Keep distance from other people's bodily fluids and blood.
- Avoiding sedimentary lifestyles and fat-laden diets, which lead to obesity and non-alcoholic liver disease.
Frequently asked questions
How to cure jaundice disease?
Jaundice usually doesn't require treatment in adults, but the causes and complications of jaundice can be treated. In infants, it is a more severe problem that can be treated by phototherapy, pharmacological agents such as intravenous immunoglobulins, and an exchange transfusion for unconjugated jaundice. For conjugated jaundice, surgical intervention such as biliary atresia is the best option.
Which organ is affected by jaundice disease?
In jaundice, the liver is the affected organ. A person suffers from jaundice when the bile duct is obstructed and the bile juice released from the liver does not reach the intestine. This unexcreted bile juice is absorbed by the blood instead of going to the duodenum. As a result, one of the most noticeable symptoms of jaundice is yellowing of the skin and eyes.
What level of jaundice is dangerous in adults?
The normal values of bilirubin depend on the age, gender, and health. Normal bilirubin levels are generally less than 1 milligram per deciliter (mg/dL). Adults with jaundice generally have bilirubin levels greater than 2.5 mg/dL. If the bilirubin levels are more than 3 mg/dL the patient will have scleral icterus (yellow discoloration of the eye sclera), considered as dangerous.
How long can you live with jaundice disease?
The intensity of jaundice relies on the severity of the underlying liver condition. In neonates, jaundice typically occurs due to unconjugated hyperbilirubinemia, can cross the blood-brain barrier causing a life-threatening kernicterus or bilirubin-induced encephalopathy. Obstructive jaundice is uncommon, and deaths in the first weeks of the disease's progression are extremely unusual. Occlusion of the common bile duct typically causes rapid deterioration and death in patients after a period of four to six months.
How long does jaundice last in adults?
In adults, the jaundice is caused by underlying disease conditions. The duration of the jaundice depends on the severity of the liver disease. In general, it may take about 10 to 14 days to recover from the signs and symptoms of jaundice, but it may take about a month to recover completely. For severe or chronic disease like hepatitis, it might take 6 months to recover completely.
What is surgical jaundice disease?
It is also known as obstructive jaundice, which occurs due to conjugated hyperbilirubinemia. It is caused by a bile flow hindrance produced by a partial or total obstruction of the extrahepatic biliary route between the liver and the duodenum that require surgical treatment of jaundice disease.
How to check jaundice in blood report?
Bilirubin test is done using a blood sample. Total, indirect, and direct bilirubin are the three possible outcomes of a bilirubin test. Direct bilirubin and indirect bilirubin are added together to make total bilirubin. Direct and total bilirubin readings are included in the blood report.
For adults, a total bilirubin test of 1.2 mg/dL is considered normal, while a reading of 1 mg/dL is considered normal for people under the age of 18, and a reading of 0.3 mg/dL is considered normal for both age groups. Women and children may have modest variations, and these findings may be affected by diet, medication, or strenuous physical activity. An increase in the normal levels of direct and total bilirubin suggests the presence of jaundice or other liver problems.
What are the diagnostic tests for jaundice or hyperbilirubinemia?
Diagnostic procedures for hyperbilirubinemia may include, increase or decrease in liver enzymes such as AST, ALT, and ALP, and gamma-glutamyl transferase levels, which provide information on the functionality of the liver; an increase in direct and indirect bilirubin levels that reveal the condition of hyperbilirubinemia; and a complete blood count that may provide information on the red blood cell count and reticulocyte count.
In addition to this, the gastroenterologist might suggest serological, imaging and endoscopy tests to rule out the causative factor for hyperbilirubinemia or jaundice.
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.