Pharyngeal cancer - Causes, Symptoms, Stages, Prognosis, Risk Factors
Pharyngeal cancer definition
When healthy cells multiply out of control, forming a tumour (a mass of cells) which could be cancerous or benign. If cancer begins in the pharyngeal areas, it is called pharyngeal cancer.
The oropharynx, oral cavity and other parts of the head and neck provide the ability to chew, swallow, breathe, and talk. The pharynx begins after the oral cavity. It includes the following:
- Tonsils
- The base of the tongue
- Soft palate
- Part of the throat behind the mouth

Types of pharyngeal cancers
The site of cancer origin distinguishes the basis of the types of pharyngeal cancer. The most common pharyngeal cancer sites are:
- The nasopharynx (the upper throat situated on the back of the nose).
- The oropharynx, which includes:
- The middle throat behind the mouth.
- The back part of the tongue (last 1/3rd of the tongue)
- The soft palate (the back of the roof of the mouth), including the uvula.
- The back and side walls of the throat.
- The tonsils.
- The hypopharynx (the lower bottom part of the throat).
Posterior pharyngeal wall cancers are one of the rare hypopharyngeal cancers, accounting for around 7%. Silent during the early stages, the posterior pharyngeal wall cancers majorly are presented in their advanced stage. Even though the cervical vertebral bodies are close to the Posterior pharyngeal wall cancers, direct invasion of the cervical vertebrae is rare.
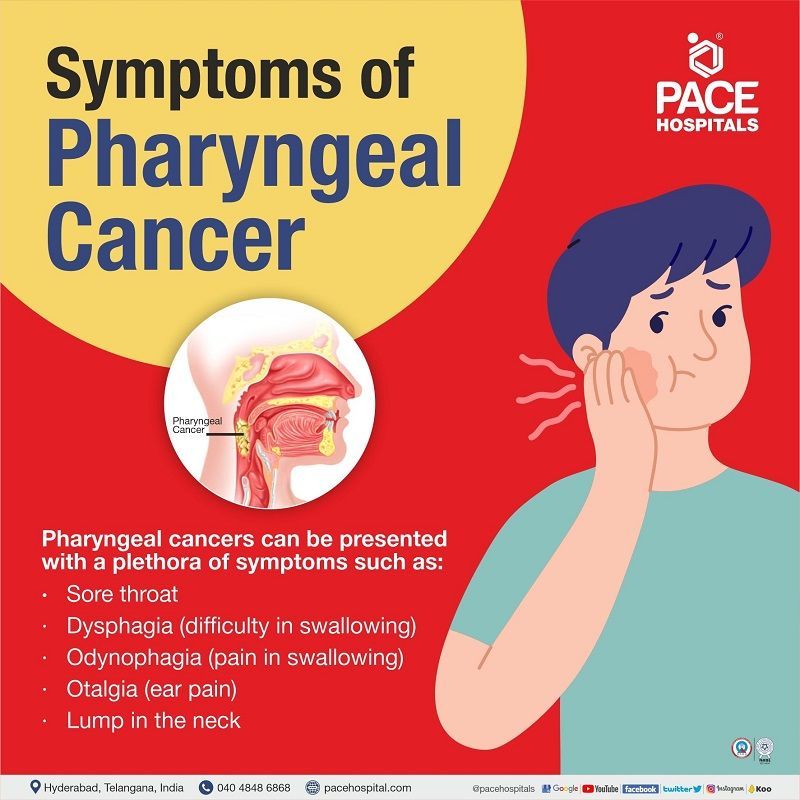
Pharyngeal cancer symptoms
Pharyngeal cancers can be presented with a plethora of symptoms which vary by the tumour’s location, such as high-pitched sounds during breathing or hoarseness in laryngopharyngeal cancer. Despite the location, a few of the most common symptoms include:
- Sore throat
- Dysphagia (difficulty in swallowing)
- Odynophagia (pain in swallowing)
- Dysarthria (slowed/slurred speech due to weakness in the muscles creating speech)
- Lump in the neck
- Otalgia (ear pain)
- Voice changes (hoarseness)
- Unexplained weight loss
- Hematemesis (blood vomiting)
- Ulcer in the oropharyngeal area
The symptoms could also present a red or white patch on the
- Base or posterior one-third of the tongue
- Posterior and lateral pharyngeal walls
- Soft palate
- Tonsils
Chronic pharyngitis cancer: Throat cancer can cause chronic painful throats in rare cases, which begins in the pharynx or larynx (voice box). Shortness of breath, lumps in the neck, or bleeding in your nose or mouth may occur as a result of the throat pain. Posterior pharyngeal wall cancer symptoms are also the same as the above explained.
Pharyngeal pouch cancer: The pharyngeal pouch cancer symptoms could range from weeks to years, presenting weight loss, regurgitation of undigested food, fetor ex ore (strong evil-smelling odour), borborygmi in the cervical region (borborygmus is the rumbling or gurgling noise due to fluid and gas movement in the intestines.), coughing.
Nevertheless, at times the patients remain asymptotic, and the discovery of pharyngeal cancer is not made until it reaches an advanced stage.
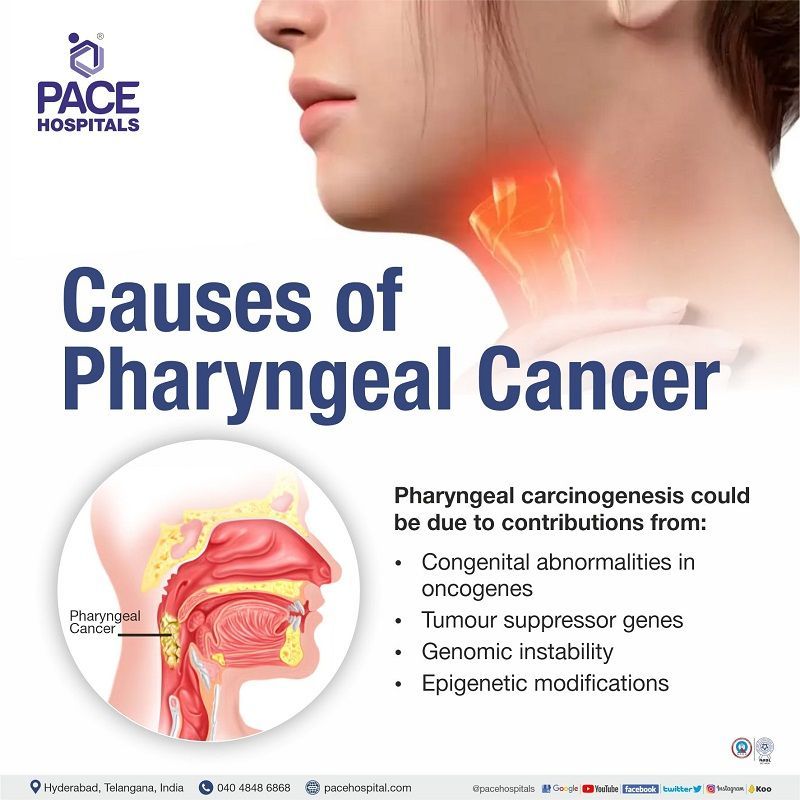
Pharyngeal cancer causes
Pharyngeal carcinogenesis, like other cancers, progresses from dysplasia to invasive phenotypes. Genetic and proteomic approaches have revealed molecular pathology such as congenital abnormalities in
- Oncogenes
- Tumour suppressor genes
- Genomic instability
- Epigenetic modifications.
Various risk factors could play a key role in enhancing the aforementioned genetic abnormalities.
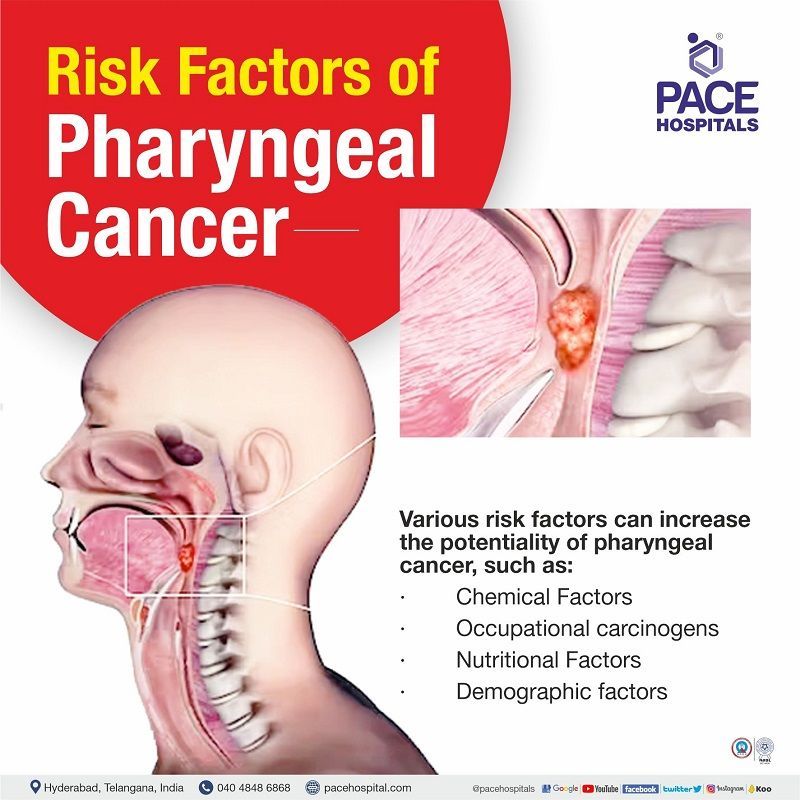
Pharyngeal cancer risk factors
Various risk factors can increase the potentiality of pharyngeal cancer, such as:
- Chemical Factors
- Occupational carcinogens
- Nutritional Factors
Chemical Factors
- Tobacco - There are ample amounts of evidence demonstrating that the consumption of tobacco in various forms, including (smoking, chewing, and in betel quid) could have a carcinogenic impact on the pharyngeal cavity, with smoking being the most standard form of tobacco use (cigarettes, cigars, pipe and bidi, hookah or chillum). In some parts of India (Mizoram and other northeast regions.), tobacco smoke is dissolved in water ("smoke on the water"), which is another peculiar form of tobacco use.
- Alcohol - Multiple studies have linked alcoholism to oral cancers and pharyngeal cancers, and it is exceptionally high in people indulging in alcoholism and tobacco use. Individuals consuming more than 170g of whiskey/day demonstrate ten times increased risk of oral cancer.
- Marijuana - studies showed the increased average risk for patients using marijuana.
Occupational carcinogens
- Formaldehyde - Hypopharyngeal and nasopharyngeal cancers can be increased with repeated exposure to formaldehyde.
- Asbestos –Studies demonstrated an increased risk for oral and pharyngeal cancers, including pharynx and hypopharynx.
- Wood particles - A reported a 5-fold and 4-fold risk for oral cavity and oropharyngeal cancer was seen among subjects exposed to wood particles.
- Metal particles-A 2006 study evaluated 20 occupational substances, including metal dust and demonstrated an increased associated risk with nasopharyngeal cancer.
- Coal particles- Association of occupational exposure to coal dust is seen with the development of hypopharyngeal cancer but not for other anatomical cancer sites.
- Smoke and fumes from different sources- An increased risk of oral and pharyngeal cancer is seen after >8 years of occupational exposure to welding fumes. Increased risk of nasopharyngeal cancer is seen with exposure to fumes from different sources (cooking, engines, wood, etc.), proportional to intensity.
Nutritional Factors
- Dietary deficits may potentially cause pharyngeal cancer. A reduced risk can be seen with a diet rich in fruits and vegetables.
Pharyngeal cancer diagnosis
While there are various diagnostic tests to identify confirm the ailment, not every individual necessarily needs to undergo every test. The oncologist and the healthcare team discuss within themselves before prescribing any of the tests outlined here.
- Endoscopy
- Laryngoscopy to examine the larynx,
- Pharynxgoscopy to investigate the pharynx,
- Nasopharyngoscopy to check the nasopharynx and other connecting cavities.
- Radiography: It is usually done to assess the bony invasion dental assessment.
- Ultrasonography: Ultrasonography is done during needle biopsy (both with or without needle biopsy)
- Magnetic Resonance Imaging (MRI): It gives perfect visualisation of the cancer
- Computed Tomography (CT): The size of the tumour can be estimated with a CT scan
- Positron Emission Tomography (PET): PET combined with a CT scan can detectthe recurrence of the primary tumours.
- Biopsy: A biopsy can collect a sample of the tissue for further examination.
Pharyngeal cancer treatment
The primary treatment options for oral or oropharyngeal cancer are surgery, radiation therapy, medication-based, and comprehensive dental treatment.
Surgery
- Maxillectomy hard palate (roof of the mouth) removal.
- Neck dissection (done to prevent the spread of cancer to neck lymph nodes)
- Laryngectomy (removal of the larynx - voice box)
- Transoral robotic surgery (TORS) and transoral laser microsurgery (TLM): both are minimally invasive surgeries
Radiation therapy
- High energy X-rays or other types of radiation are utilised to kill cancer cells and their growth.
Chemotherapy
- Medicines are given along with radiation therapy to kill growing cancer cells. Targeted therapy and immunotherapy are other kinds of therapy given to treat cancer.
Frequently Asked Questions - FAQs
-
Can pharyngitis cause cancer?
Yes. Pharyngitis can cause cancer if it is misdiagnosed or improperly treated. Pharyngitis treatment requires time, and patients frequently tend to discontinue their medication when their symptoms improve, causing the sore throat to become chronic. This is a classic case of medication non-adherence. The prognosis of pharyngitis could lead to severe consequences such as nasopharyngeal cancer in case of improper diagnosis or ineffective treatment.
-
Can granular pharyngitis cause cancer?
Yes. Long-standing pharyngitis can cause cancer if it is misdiagnosed or improperly treated. Chronic granular pharyngitis is the altered pharynx mucous membrane.
-
What throat disease can lead to cancer?
In recent years, an increased incidence is seen in the occurrences of throat cancer in persons who have had specific viral infections, such as human papillomavirus (HPV), a prevalent sexually transmitted illness, and the Epstein-Barr virus, which causes "mono." Pharyngeal cancer occurs more frequently than laryngeal cancer.
-
Is pharynx cancer curable?
Yes. Oropharyngeal cancers can be cured, especially if it is diagnosed at an early stage. Although, treating the cancer is the primary goal, the treatment also involves the salvage of functioning of the nearby nerves, organs, and tissues is also very important.
-
Is throat cancer curable?
Yes. Throat cancer can be cured when found early. About half of cancer patients can be cured if the cancer hasn't spread to nearby tissues or lymph nodes in the neck. If the cancer has spread (metastasis) to lymph nodes and various body parts other than the head and neck, treatment can be a little tricky.
-
What is the age range for throat cancer?
Usually, a throat cancer diagnosis is made between the ages of 55-64. Patients with laryngeal cancer are frequently over the age of 55, culminating with an average age of 66. Men are more likely than women to die from laryngeal cancer.
-
Can you still eat with throat cancer?
A feeding tube may be necessary for food intake. While tiny quantities of food (such as soft or pureed foods and fluids) may be able to be consumed with the eventual healing of throat cancer, the patients will be able to increase their food intake, and the doctor will eventually remove the feeding tube.
-
What is Stage 1 early throat cancer?
Stage I throat cancer measures no bigger than 2 cm (about 1 inch) and hasn't spread to nearby lymph nodes. Cancers of the throat that are caught early are small, localised, and usually treatable with surgery and/or radiation therapy. Cancers in stages I are in the early stage.
-
What are the survival rates for nasopharyngeal cancer?
The nasopharyngeal cancer survival rates are based on the extent of the growth and its spread before diagnosis. Basically, the five-year survival rate for nasopharyngeal cancer is 61%, but delving deeper into the three survival rates seen in nasopharyngeal cancer, the rates are:
- Localised: No tumour spread beyond the tissue in which it developed– 85%
- Regional: Cancer spread to nearby tissues or lymph nodes – 71%
- Distant: Cancer spread to farther parts of the body - 49%
-
What are the survival rates for oropharyngeal cancer?
The oropharyngeal cancer survival rates are based on the extent of the growth and its spread before diagnosis. The five-year survival rate for oropharyngeal cancer is 49%, but delving deeper into the three survival rates seen in oropharyngeal cancer, the rates are as follows:
- Localised: No cancer spread beyond the tissue in which it developed – 62%
- Regional: Cancer spread to nearby tissues or lymph nodes – 57%
- Distant: Cancer spread to farther parts of the body - 29%
-
What are the survival rates for laryngopharyngeal cancer?
The laryngopharyngeal cancer survival rates are based on the extent of the growth and its spread before diagnosis. The five-year survival rate for laryngopharyngeal cancer is 49%, but delving deeper into the three survival rates seen in laryngopharyngeal cancer, the rates are as follows:
- Localised: No tumour spread beyond the tissue in which it developed – 61%
- Regional: Cancer spread to nearby tissues or lymph nodes – 47%
- Distant: Cancer spread to farther parts of the body - 31%
-
What are the survival rates for hypopharyngeal cancer?
The hypopharyngeal cancer survival rates are based on the extent of the growth and its spread before diagnosis. The five-year survival rate for hypopharyngeal cancer is 32%, but delving deeper into the three survival rates seen in hypopharyngeal cancer, the rates are as follows:
- Localised: No cancer spread beyond the tissue in which it developed – 52%
- Regional: Cancer spread to nearby tissues or lymph nodes – 34%
- Distant: Cancer spread to farther parts of the body - 23%
Related article:
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 8977889778
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.