Uterine Artery Embolization: Procedure, Success Rate, Recovery & Cost
At PACE Hospitals, a team of Interventional radiologists and surgeons are experienced in treating cases of symptomatic uterine fibroids or leiomyomas or myomas with using advanced interventional techniques involving laser treatment with minimal time and high success rate.
We have a team of the best doctor for uterine artery embolization in Hyderabad, they are having extensive experience in performing uterine fibroid embolization – UFE.
Request an appointment for Uterine Fibroid Embolization
Uterine Fibroid Embolization - appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 7842171717
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
Whatsapp: 7842171717
Regards,
Pace Hospitals
Hitech City and Madinaguda
Hyderabad, Telangana, India.
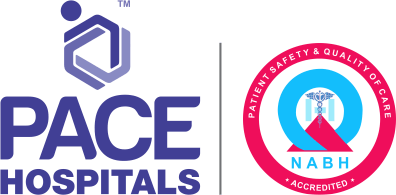
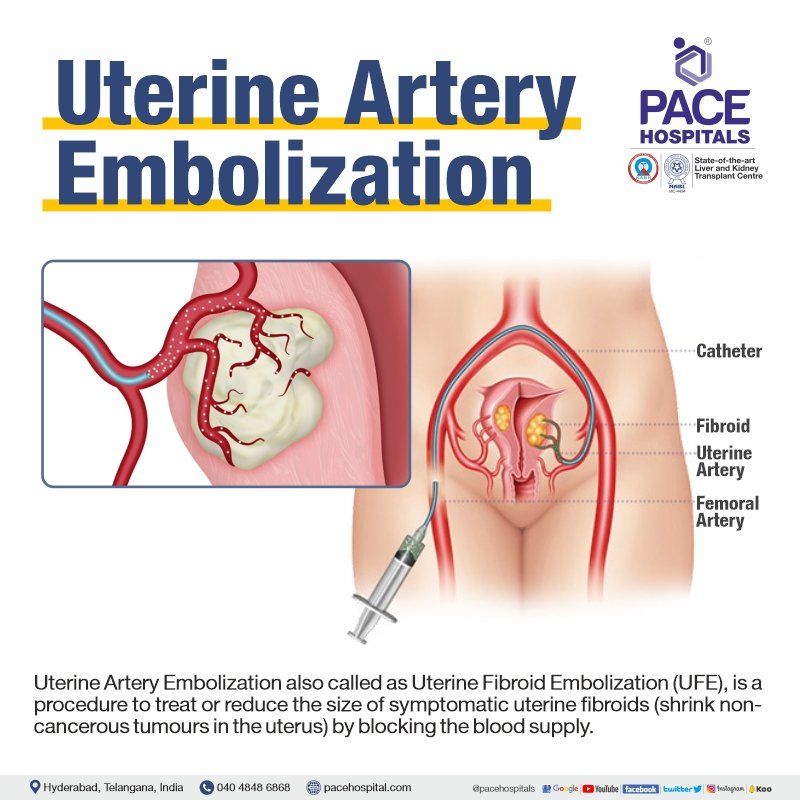
What is Uterine Artery Embolization and its purpose?
Uterine Artery Embolization also called Uterine Fibroid Embolization (UFE), is a procedure to treat or reduce the size of symptomatic uterine fibroids (shrink non-cancerous tumours in the uterus) by blocking the blood supply.
Monitoring through fluoroscopy (a form of real-time x-ray) the embolic agents (agents for blocking blood flow) are delivered to the uterus to treat the fibroids. The duration of recovery and hospitalization are minimal as this procedure is not a major surgery.
Uterine artery embolization is also a safe and reliable procedure for the postpartum haemorrhage (blood loss by the mother during birth).
Uterine artery embolization is one of the procedures in which the uterus of the patient is kept intact, thereby giving her a chance to have biological children in the future.
What are the indications of Uterine Artery Embolization?
There are various types of uterine fibroid patient groups suffering with several underlying and associated conditions in whom the differentiation of opting uterine artery embolization and the other surgical procedures is necessary.
The entire indications list of uterine artery embolization or uterine fibroid embolization (UFE) include:
- intramural fibroids (fibroids growing within the muscular uterine wall)
- menorrhagia (menstrual periods with abnormally heavy or prolonged bleeding)
- pelvic pain and pressure symptoms
- bladder outlet obstruction and hydronephrosis (swelling of a kidney due to a build-up of urine because of a blockage or obstruction)
- fibroids with otherwise undiagnosed infertility
- as a preoperative measure for large fibroids
- dysfunctional uterine bleeding
- adenomyosis (endometrial tissue exists within and grows into the uterine wall)
Usually, the ideal patients for uterine fibroid embolization are those patients’ groups in whom surgery is contraindicated. The ideal candidates include:
- The patients with substantial health problems such as morbid obesity, diabetes, hypertension, etc can be very poor candidates for anaesthesia and any major surgery
- Uterine artery embolization can also be used as a preoperative treatment for patients with very large uteri scheduled for myomectomy to reduce uterine size, intra-operative blood loss, and correct anaemia.
- Patients with rare blood groups and who will not accept transfusion are also excellent candidates for uterine artery embolization.
The less ideal candidates include:
- Patient with small uterus (<600 cc)
- Patient with just a single fibroid
- Patients suffering with a resectable submucous fibroid
- Patients suffering a single fundal fibroid which can be easily removed by laparoscopy.
Contraindications of Uterine Artery Embolization
The contraindications to uterine fibroid embolization rarely arise. They are:
- Pregnancy patients suffering with fibroids
- Postmenopausal women
- Patients with severe contrast allergy
- Patients with renal (kidney) failure
- Patients suffering with uterine arteriovenous malformation (abnormal and non-functional connections between the uterine arteries and veins)
- Patients with unknown pelvic mass
Considerations of interventional radiologist before opting a uterine artery embolization
Although the primary duty of an interventional radiologist is to treat the patients with uterine fibroids, his attention towards the wishes and aspirations of the patients are regarded paramount.
The considerations of an interventional radiologist include not only in the avoidance of Uterine Artery Surgery or its adverse effects but also in retaining the fertility of the patient by preserving the uterus, especially when any patient intends to experience parturiency (motherhood) with biological children in the future.
It is during these scenarios that the role of a doctor extent not only in weighing the medical indications and contraindications among patient groups, but also in the contemplation of the common considerations of future pregnancy when uterine artery embolization is opted.
The common considerations of uterine artery embolization which could affect future pregnancy include:
- Compromised blood supply to the uterus
- Compromised myometrial integrity and
- Premature ovarian failure
The contraindications to uterine fibroid embolization are also thoroughly discussed with the doctor which could include any of the following:
- Active infection,
- Active bleeding,
- History of pelvic irradiation,
- Life-threatening contrast allergy,
- Poorly controlled diabetes, and
- Abnormal kidney functions
Nearly all patients experience pelvic pain following uterine artery embolization, but the pain is subjective in terms of the amount and duration of post-procedural symptoms. The treating gynaecologist takes careful attention to compassionate periprocedural patient care in treating the patients and recommending this treatment option to other patients.
The interventional radiologist discusses the following pain related topics with the patients:
- The expected amount and time course of pain after uterine artery embolization, and finding out the controllable intra-procedural factors influencing post-procedural symptoms;
- Differentiating the deviations from the usual pattern which raise suspicion for potential complications
- Development of a pain management protocol for the procedure, the in-hospital post-procedure period, and the outpatient recovery period
- Addressal of commonly associated symptoms such as nausea, vomiting, constipation, and fever
As a consequence, if this procedure is to be offered to young women wishing future pregnancy, it is the responsibility of the doctor to provide a full and complete information about the potential risks as wells as the advantages before offering the informed consent form.
Preparing for uterine artery embolization
Diagnostic imaging is likely to be the first method used by the doctor for the assessment of the condition. Usually, MRI is the preferred procedure, but laparoscopy could also be utilised by the primary care doctor for a direct look at the uterus.
- During the discussion the patient is expected to reveal any recent illnesses, medical conditions, allergies, and medications (including herbal supplements with the gynaecologist).
- Interventional radiologist may ask the patient to discontinue any blood thinners, non-steroidal anti-inflammatory drugs (NSAIDs), and other medications that could reduce inflammation a few days before surgery.
- Patients should always inform their interventional radiologist and technician if they are pregnant, as it can help the healthcare personnel in protecting the developing fetus from any unnecessary radiation exposure.
- Depending upon the healthcare organization the patients may be asked to stay overnight at the hospital before the procedure.
- It may be necessary for the patient to fast from midnight on the night before the commencement of the procedure.
- Patients are advised to leave the jewellery at home, and a hospital gown may be provided before the procedure.
During uterine artery embolization
One of the advantages of uterine artery embolization is the fact that it is a minimally invasive procedure, which is routinely performed without the need for general anaesthesia. Most interventional radiologists use a combination of narcotics and benzodiazepines for conscious sedation, however there are some who use spinal analgesia.
- It takes about 90 minutes to finish this procedure.
- Either in a cath lab or occasionally in an operating room the procedure is planned.
- The patient is made to lie down in a supine position (lying on the back) on the procedure table.
- Electrodes for the monitoring of heart rate, blood pressure, oxygen level, and pulse are connected to the body
- A sedative will be administered through an intravenous line inserted into a vein in the hand or arm (opioid analgesic agent and a short-acting anxiolytic/sedative could be given with an NSAID). A breathing tube is attached only when necessary.
- A local anaesthetic is injected to numb the area after sterilizing the site (femoral artery at the groin area) followed by a tiny incision made in the skin.
- The catheter is inserted into the femoral artery in the groin area under x-ray guidance (fluoroscopy). The catheter can be guided more easily into the uterine arteries with the help of a contrast material.
- Once the catheter is in place, an arteriogram of the uterine artery is performed through which the distribution, and speed of flow, and to exclude any unusual occurrences such as arterio-venous malformation of the uterus.
- The embolization can then be performed. By moving the catheter to a new location, the embolic agents such as gelatine sponge, polyvinyl alcohol (PVA) powder, and calibrated tris-acryl microspheres can be injected into either the right or left uterine artery.
- The embolic material is suspended in dilute contrast and injected into the uterine artery.
- It is carried into the uterus by blood flow and causes occlusion of the vessels by a combination of physical occlusion and thrombus (blood clot) formation.
- After the first uterine artery has been embolized, the other uterine artery is then selectively catheterized and embolized in the same fashion.
After Uterine artery embolization
Depending upon the healthcare organization the patient may be needed to stay in the hospital and discharged to return home the day after the procedure
- Sedation during medical procedures typically results in the patient feeling calm, sleepy, and at ease. The waking up of the patient depends on the extent of sedation.
- Mild pelvic cramps, nausea, and a low-grade fever could be seen for several days but gradually subsides over the next few days.
- Pain medication is given which effectively alleviates any suffering.
- A laxative could also be provided as the opioid narcotics which were given during the procedure could cause constipation
- Several days of light to moderate vaginal bleeding is possible. To determine the extent of drainage sanitary pads usage must be maintained which is examined by the interventional radiologist during the follow-up.
- Exercises for coughing and deep breathing will be taught.
- A few hours after the procedure, the patient may be given fluids to drink and gradually solid foods can also be consumed.
- The groin incision must be maintained clean and dry and specific bathing instructions by the interventional radiologist must be followed.
- Strenuous activity must be avoided and walking may be recommended.
- Fibre and plenty of fluids must be consumed to avoid constipation as straining for a bowel movement is not desirable may cause problems.
- Usually, women can be assessed for their need for further treatment, three to six months after uterine artery embolization. Women with persistent symptoms can be offered surgery.
-
Is uterine artery embolization a safe procedure?
Uterine artery embolization or Uterine fibroid embolization (UFE) is a safe and reliable procedure for the female patients those who all are having bleeding problems due to cancerous tumors, uterine fibroids, childbirth, trauma and other conditions.
-
What is the uterine fibroid embolization success rate?
Uterine artery embolization or Uterine fibroid embolization (UFE) is a effective and safe surgery in patients with having symptomatic uterine fibroids and recorded nearly 92% success rate based on the recent studies. UFE is the preferred procedure over other procedures as the uterus remains intact which is the main organ for conceiving and having biological children in female.
-
How painful is the uterine fibroid embolization?
After uterine fibroid embolization (UFE) females may have cramping pain in their lower abdomen for 5 to 7 days or more, during this time they can have uncomfortable, queasy feelings and may have irregular or missed periods. Some of them may notice vaginal bleeding and discharge for 20 to 30 days. Incase of persistent pain and bleeding it is advised to consult primary care doctor.
-
What is the impact on fertility after uterine artery embolization?
The impact of uterine artery embolization or uterine fibroid embolization (UFE) on fertility after treating uterine fibroids, has mixed results. A 2018 systematic review demonstrated that around 50% of the women became pregnant after uterine artery embolization or uterine fibroid embolization (UFE) while the average pregnancy rate remained 29%. Around 64% of pregnancies ended in miscarriage.
Uterine Fibroid Embolization Side effects and complications
Although uterine artery embolization has been introduced as an alternative to avoid the risks associated with hysterectomy or myomectomy, it has got its own set of side effects and complications which can be classified into intra-operative and postoperative complications. Majority of the complications are rare and are experienced by less than 1% of patients.
Intra-operative risks and complications
- Puncture site complications: Infection, bleeding, and hematoma (pool of clotted blood) formation at the groin puncture site have been reported to occur at a frequency of less than 1%. Bleeding is usually managed by applying pressure while in the recovery room patients are instructed to keep their legs straight for four to six hours, and to refrain from coughing.
- Allergic/anaphylactic reactions: Allergies to the iodinated contrast dye and to medications given for sedation and analgesia (pain management) can occur and they range from mild to life-threatening events. Allergic reactions are encountered by about 1% of patients.
- Misembolization: refers to a situation when embolic agents especially (polyvinyl alcohol particles) go to other organs unintentionally. Although this can be a serious problem it is extremely rare event. Potential non-target embolization can result in ovarian dysfunction and adjacent organ ischemia or even necrosis. Arteriography can be performed by the gynaecologist to minimize the risk for misembolization, by confirming the safe catheter position that no vascular anomalies or aberrant vessels are present.
- Radiation exposure: The average time for uterine artery embolization has been reported to be approximately one hour. However, the median fluoroscopy time required to complete the procedure is 15-30 minutes.
Post-procedure side effects and complications
- Acute post-embolization pain: Catheterization of the artery can cause ischemia (low blood supply) of the uterus and fibroids which is by far the most painful factor post-embolization. Preemptive analgesia (treatment that is initiated before the procedure in order to reduce pain) can help reduce the pain.
- Post-embolization syndrome: About 40% of patients experience a variety of signs and symptoms such as abdominal pain, malaise (general feeling of discomfort, illness, or lack of well-being), anorexia (loss of appetite), nausea, vomiting, low-grade fever, and leucocytosis (increased white cells in the blood indicative of an infection.) which is experienced by approximately one-third of the patients. The syndrome is self-limiting and usually resolves within 48 hours with supportive of intravenous fluids of painkillers. Antibiotics may be prescribed for the low-grade fever.
- Infection: Incidence of febrile morbidity (temperature rise above 100.40 F lasting about or more than 24 hours) and sepsis (serious condition due to harmful microbes in the blood/tissues, potentially leading to the malfunctioning of various organs, shock, and death.) following embolization has been reported to be between 1-1.8%. The infections can be treated with prophylactic antibiotics.
- Ovarian dysfunction: Temporary and permanent menopausal symptoms indicative of ovarian failure have been reported by up to 5% of women after the procedure. Reasons are not clearly elucidated. Ovarian failure can be seen in:
- Older patients (> 45 years of age)
- Greater exposure to radiation
- Misembolization etc
- Menstrual dysfunction: Amenorrhea (abnormal absence of menstruation) after embolotherapy is highly age dependent. The rate increased gradually to a 10% by the age of 50 years and jumped to over 40% after the age of 50. Permanent amenorrhea is a major complication in women desiring parturiency. No significant change or worsening of menstrual bleeding after the procedure is seen in a very small percentage of the patients
- Transcervical myoma expulsion: Spontaneous expulsion of the fibroids through the cervix has been reported to occur in approximately 5-7% of patients
- Uterine wall integrity: Uterine wall defects, uterine necrosis (death of tissue) following embolization could be seen. In patients contemplating pregnancy the integrity and features of the uterine wall and cavity should be assessed by laparoscopy and hysteroscopy prior to undertaking pregnancy.
Frequently asked questions:
What is Uterine artery embolization in PPH - postpartum hemorrhage?
Uterine artery embolization or Uterine fibroid embolization (UFE) in postpartum haemorrhage (blood loss by the mother during birth) is used for stopping vaginal bleeding. Among uterine artery embolization patients for postpartum haemorrhage (PPH), a 96% of cases were successful with very few patients contracting any complications.
What are the uterine artery embolization pregnancy risks?
The complications of uterine artery embolization or Uterine fibroid embolization (UFE) with respect to pregnancy include: prematurity, intrauterine growth restriction, abnormal placentation, and increased likelihood of cesarean delivery (C-section). Nevertheless, uterine artery embolization is the preferred method to other procedures such as hysterectomy as the uterus remains intact in this procedure, which is the prime organ for conceiving and having biological children. On the other hand, it must be understood that uterine artery embolization comes with its own pros and cons.
What is the uterine artery embolization recovery time?
Uterine artery embolization duration of recovery and hospitalization are minimal, recovery will take nearly 5 to 7 days as uterine fibroid embolization (UFE) procedure is not a major surgery, after 10 to 15 days patients can start their normal activities. Right after the procedure:
- Mild pelvic cramps, nausea, and a low-grade fever could be seen for several days but gradually subsides over the next few days.
- Pain medication is given which effectively alleviates any suffering.
- A laxative could also be provided as the opioid narcotics which were given during the procedure could cause constipation.
What is the uterine artery embolization success rate for adenomyosis?
The long-term studies of uterine artery embolization or uterine fibroid embolization (UFE) in the treatment of adenomyosis showed fewer promising results. A 2007 study demonstrated a 57.4% success rate after 58.8 months of the therapy. Another 2005 study displayed a clinical success rate of 56% in nine women at 24 months. Adenomyosis was formerly thought to be a contraindication with uterine artery embolization, but recent studies demonstrated the efficacy of uterine artery embolization for treatment of adenomyosis.
Why there is irregular or no period after uterine artery embolization?
Ovarian and menstrual dysfunction are few of the complications which can be expected in patients who underwent uterine artery embolization or uterine fibroid embolization (UFE). It is completely normal to expect missing, irregular or no period after UFE.
Temporary and permanent menopausal symptoms indicative of ovarian failure have been reported by up to 5% of women after the procedure. The rate of amenorrhea (abnormal absence of menstruation) after uterine artery embolization increased gradually to a 10% by the age of 50 years and jumped to over 40% after the age of 50.
Pregnancy after uterine artery embolization for AVM- arteriovenous malformation
Bleeding from an abnormal connection between the artery and vein in the uterus is the hallmark symptom of uterine arteriovenous malformation (AVM) which is a rare but potentially fatal condition. Embolizing a uterine arteriovenous malformation increases the risk of spontaneous abortion and foetal growth retardation, so pregnancy after embolization is extremely unusual.
There are reported cases which showed that uterine AVM embolization in a symptomatic patient not only alleviated her symptoms, but also led to a healthy pregnancy to term without any complications for either the mother or her child. Even the foetal outcome was positive.
Uterine artery embolization after C-Section (Cesarean Section)
A study was conducted in 2020 to compare immediate and long-term obstetrical outcomes of patients suffering with placenta accreta spectrum disorder (clinical situation where the placenta does not detach spontaneously after delivery and cannot be forcibly removed without causing massive and potentially life-threatening bleeding) who underwent cesarean delivery (c section) with and without uterine artery embolization. It is concluded that there is an increased risk of operative and postoperative complications when a cesarean section is performed using uterine artery embolization in women with placenta accreta spectrum disorder. However, it was understood that embolization lessens the need for hysterectomy and preserves fertility in cases of severe placental adherence.
What is the uterine fibroid embolization cost in India?
Uterine fibroid embolization or Uterine artery embolization cost in India ranges vary from Rs. 1,00,000 to Rs. 2,25,000 (Rupees one lakh to two lakh twenty five thousand). However, Uterine fibroid embolization in India, depends upon the type, size and number of fibroids, the different private hospitals in different cities.
What is the uterine fibroid embolization cost in Hyderabad?
Uterine artery embolization or Uterine fibroid embolization cost in Hyderabad ranges vary from Rs. 1,15,000 to Rs. 1,85,000 (Rupees one lakh fifteen thousand to one lakh eighty five thousand). However, cost of uterine fibroid embolization procedure depends upon the multiple factors such as the size, number and type of fibroids, risks associated with the surgery, selection of room for hospital stay, CGHS, EHS, ESI, insurance or corporate approvals for cashless facility.
Females looking for treatment of uterine fibroid embolization near me can get an instant appointment at PACE Hospitals by filling up the form - Request an appointment.
Our Locations
Subscribe to our newsletter and stay updated with the latest health information.
By clicking on subscribe now, you accept to receive communications from PACE Hospitals on email, SMS and Whatsapp.
Subscribe to PACE Hospitals News
Thank you for subscribing. Stay updated with the latest health information.
Oops, there was an error. Please try again submitting your details.
-

Payment in advance for treatment (Pay in Indian Rupees)
For Bank Transfer:-
Bank Name: HDFC
Company Name: Pace Hospitals
A/c No.50200028705218
IFSC Code: HDFC0000545
Bank Name: STATE BANK OF INDIA
Company Name: Pace Hospitals
A/c No.62206858997
IFSC Code: SBIN0020299
Scan QR Code by Any Payment App (GPay, Paytm, Phonepe, BHIM, Bank Apps, Amazon, Airtel, Truecaller, Idea, Whatsapp etc)
Call us at 04048486868
ADDRESS
PACE Hospitals
Hitech City : Beside Avasa Hotel, Pillar No. 18, Hyderabad - 500081
Madinaguda: Mythri Nagar, Beside South India Shopping, Madinaguda, Hyderabad - 500050
QUICK LINKS
Disclaimer
General information on healthcare issues is made available by PACE Hospitals through this website (www.pacehospital.com), as well as its other websites and branded social media pages. The text, videos, illustrations, photographs, quoted information, and other materials found on these websites (here by collectively referred to as "Content") are offered for informational purposes only and is neither exhaustive nor complete. Prior to forming a decision in regard to your health, consult your doctor or any another healthcare professional. PACE Hospitals does not have an obligation to update or modify the "Content" or to explain or resolve any inconsistencies therein.
The "Content" from the website of PACE Hospitals or from its branded social media pages might include any adult explicit "Content" which is deemed exclusively medical or health-related and not otherwise. Publishing material or making references to specific sources, such as to any particular therapies, goods, drugs, practises, doctors, nurses, other healthcare professionals, diagnoses or procedures is done purely for informational purposes and does not reflect any endorsement by PACE Hospitals as such.